Chapter outline

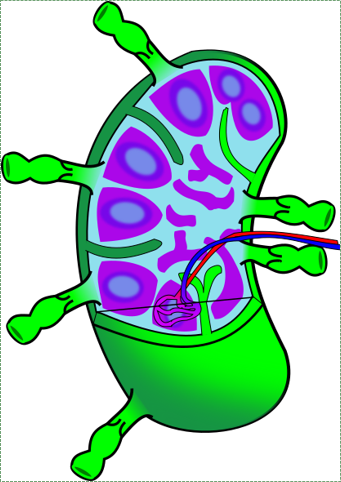
The average gland is composed of simple cuboidal epithelial cells that form grape-shaped structures called acini (although others are tube-shaped). These grape-shaped structures are where the secretions are produced. The liquids produced by these cells next enter a duct, which can be made of simple cuboidal or columnar eipthelial cells. The outside of the gland is surrounded by dense connective tissue capsule. The connective tissue extends inwards forming trabeculae (or septa), which can divide the organ into different lobes.

The mucous component of saliva helps it to adhere to all surfaces of the oral cavity. Buffers within saliva help to maintain a stable pH, despite the acidity or alkalinity of different foods, and the acidity of certain oral bacterial secretions. Buffers and electrolytes can also help disrupt the formation of bacterial biofilms, which otherwise allow bacteria to adhere to teeth. The watery nature of saliva helps to moisten food and the oral mucosa, assisting in mastication, speech and swallowing. Watery saliva helps to limit the population of oral bacteria. People swallow saliva even when they are not eating, and this flushes a percentage of oral microorganisms down to the stomach, where certain death awaits in the form of Hydrochloric Acid and a powerful protein-destroying enzyme called pepsin. The enzymes salivary amylase and lysozyme are produced by acinar cells to serve a similar purpose, breaking covalent bonds within the cell walls of viruses and bacteria. I suppose if you chewed for long enough, salivary amylase could help digest carbohydrates in food, but no one chews for long enough for that to happen. Therefore, salivary amylase should not be considered a digestive enzyme. It is an anti-microbial enzyme that helps limit oral microbiome populations.
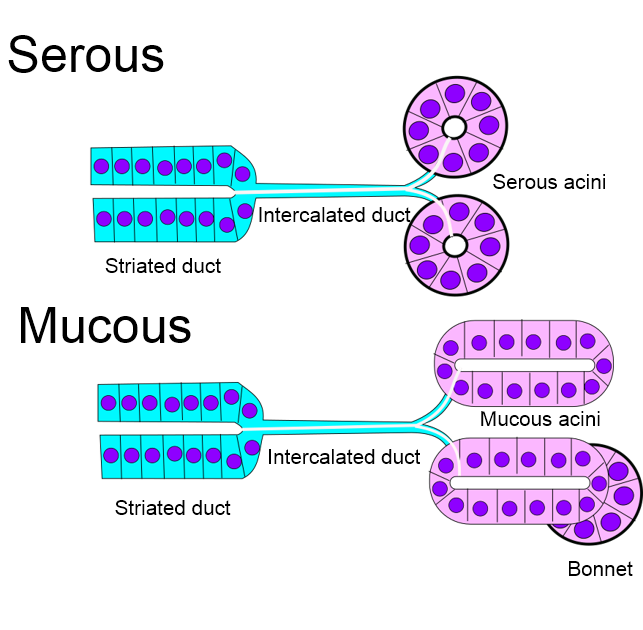
Serous acini produce more watery secretions. These are composed of simple cuboidal epithelium. Serous acini tend to stain more faintly using a traditional H&E stain, because they make fewer mucous proteins.
Mucous acini secrete more glycoproteins, making their secretion thicker and stickier. These are made of a simple columnar epithelium. Mucous acini tend to stain a little darker using a traditional H&E stain, because they make more mucous proteins.
Muco-serous acini produce secretions halfway inbetween the first two in consistency. These look like mucous acini under the microscope, with an additional bonnet of myo-epithelial cells. These cells contract like smooth muscle cells. For most epithelial cells, the actin and myosin genes are not highly expressed, except by epithelial stem cells, which may need to migrate to a different area to help repair a wound. Myo-epithelial cells, on the other hand, use some of the DNA instructions for making and organizing actin and myosin that are usually only transcribed by muscle cells, making them appear similar to smooth muscle. However, these cells have an epithelial lineage-- they differentiated from an epithelial stem cell, not from a Mesenchymal Stem Cell or myoblast.
All three secretions wind up mixing in the oral cavity to produce saliva, therefore memorizing which type of acinus does what is fairly academic. These secretions reach the oral cavity by way of different types of ducts, which can be identified under the microscope by their different type of epithelial cells. I know of no clinical significance to the types of ducts or their cells, which makes identifying the ducts by type an academic exercise. You can do it, but why would you?
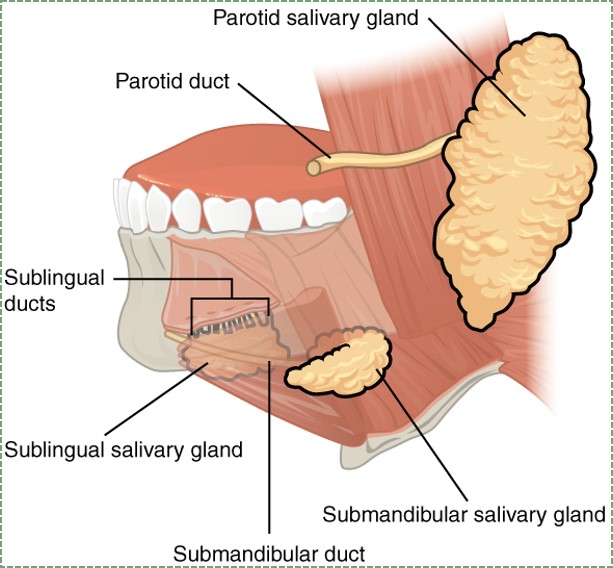
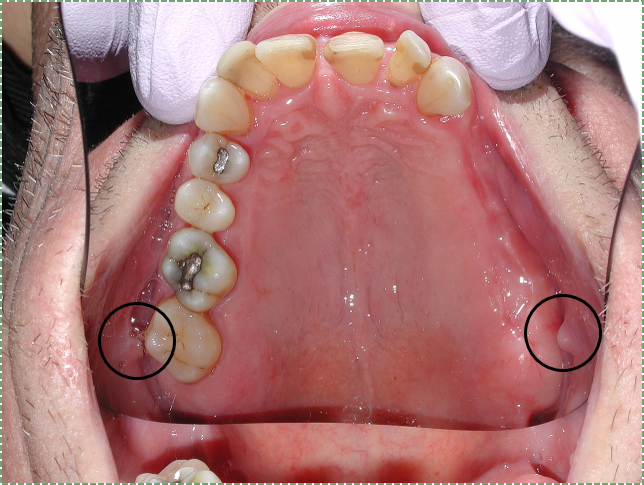
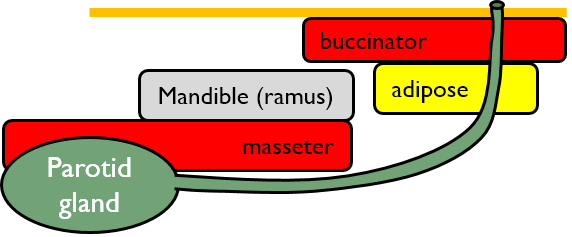
There are three major and numerous minor salivary glands. The three major salivary glands are:
| Parotid salivary glands | Largest |
| Serous (mostly) | |
| 25% saliva by volume | |
| Sub-mandibular salivary glands | 2nd largest |
| Muco-serous | |
| 65% saliva by volume | |
| Sub-lingual salivary gland | Mucous |
| 10% saliva by volume |

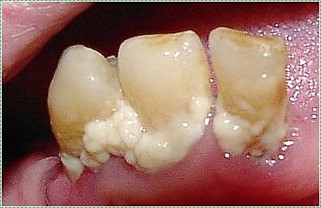
Hyposalivation, or decreased saliva production, can be caused by certain diseases, medications, cancer treatments, and aging. It may result in xerostomia, or dry mouth. Reduced saliva can decrease the healing ability of the oral mucosa, leading to sores. Reduced saliva also removes some of the limits to growth placed on the oral microbiome, leading to infections and caries. Reduced taste can also be a consequence, which patients might compensate for by flavoring their food with excessive levels of salt. Using Monosodium Glutamate (MSG) to enhance both flavor and saliva production is a significantly safer option, despite fears of the non-existant "Chinese Restaraunt Syndrome".

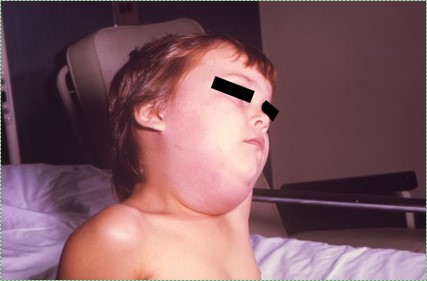
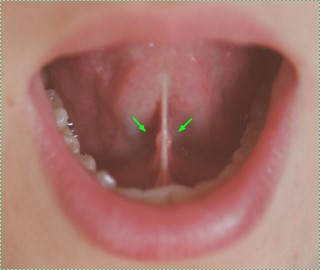
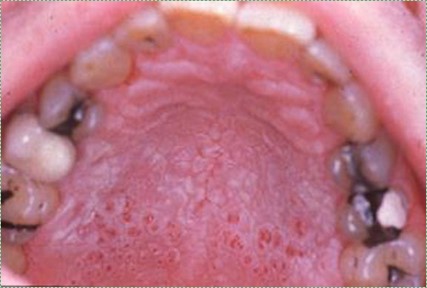
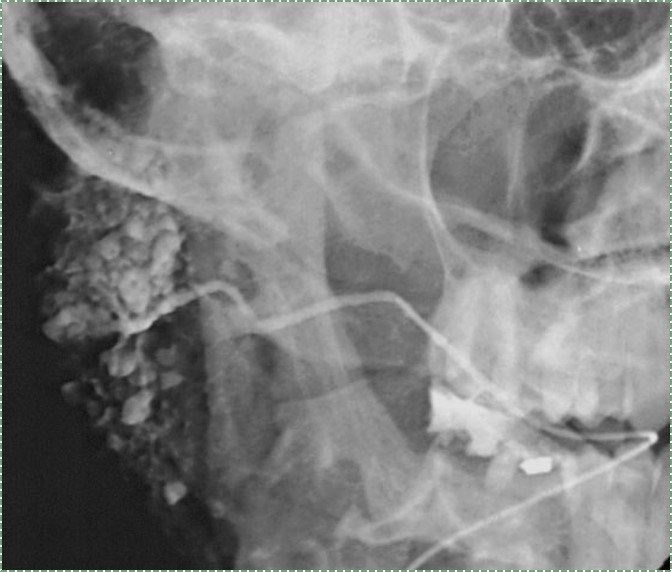
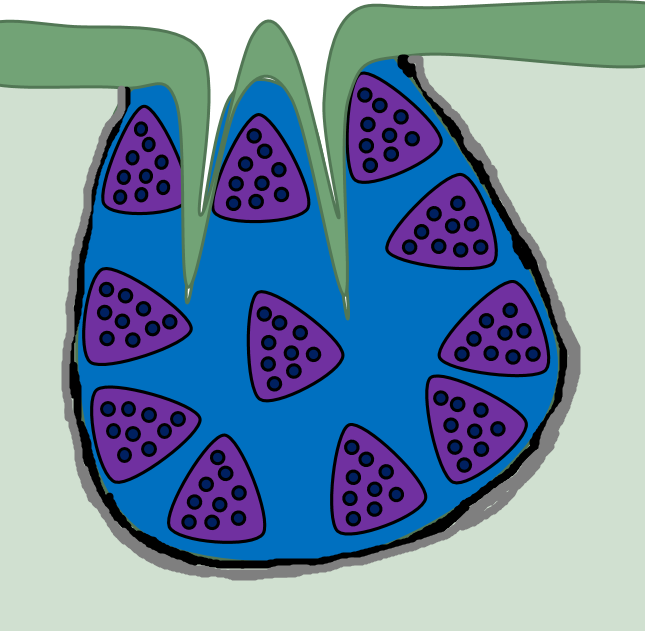
The electrolcytes in saliva can precipirate and form salivary gland stones, or sialoliths. Large sialoliths may block the duct of one of the salivary glands, which stops the secretion-- but not the production-- of saliva. As a result, saliva builds up in the gland, causing swelling and possibly inflammation. Blockage of a minor salivary gland produces a swelling within the oral mucosa known as a mucocoele, while blockage of a major salivary gland produces a ranula.
 |
 |
| Mucocoele by Dozenist is liscensed CC BY SA 3.0 | Ranula human by Ph0t0happy is liscensed CC BY SA 3.0 |
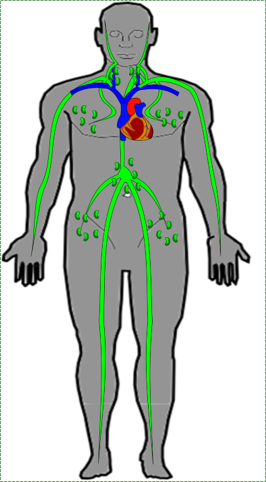
| Lymphatic vessels | Drain ECF off organs, including teeth |
| Lymph nodes | Filter debris and identify pathogens |
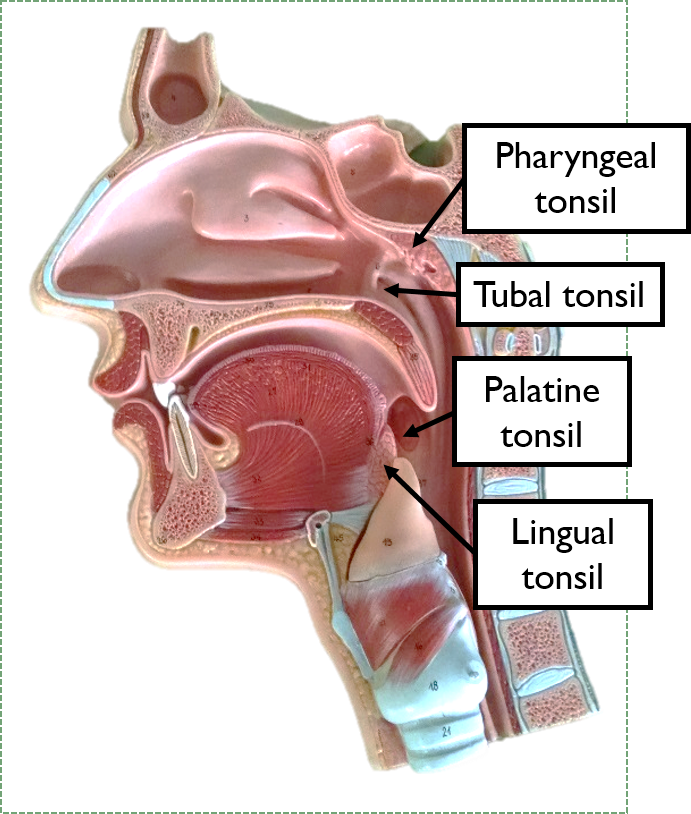
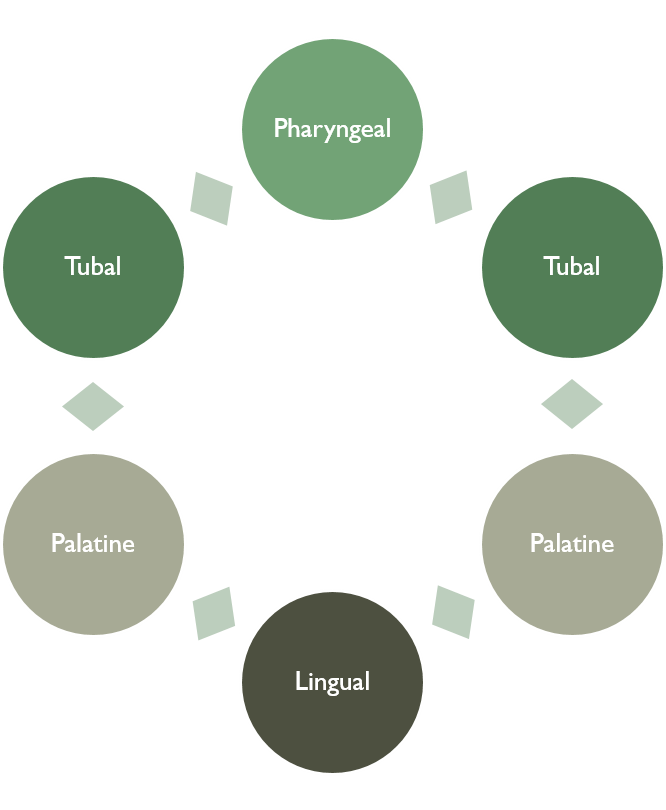
| Tonsillar tissue | Identify pathogens |
| Other lymphatic organs | Located below the neck |
"
Lymph nodes serve two major functions. One is to clear and cellular debris before lymph reaches the circulatory system, becoming blood plasma again. Two is to identify pathogens and begin an inflammatory response. If this occurs, white blood cells begin to multiply within the node and begin secreting inflammatory molecules.

In the absence of infection, lymph nodes are soft and cannot be felt. However, if the white blood cells detect a pathogen, they undergo cell division and release inflammatory molecules. This leads to lymph nodes becoming palpable, possibly visibly swollen, and likely sensitive to the touch.


Tonsillar tissue can also become inflamed. When it does, the increased number of white blood cells may be visible as white-ish patches within the inflamed tonsil(s).
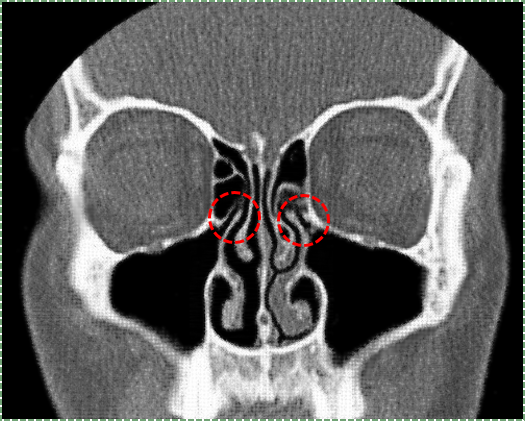
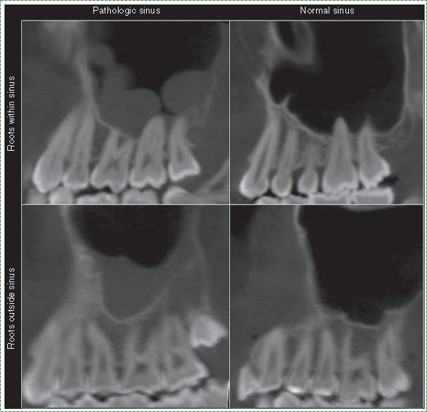
The para-nasal sinuses are spaces within the frontal, sphenoid, ethmoid and maxillary bones that surround the nasal cavity. The maxillary, frontal and spehnooid sinus connect to the nasal cavity via small passageways. The paranasal sinuses are lined with pseudostratified epithelium. This epithelium produces mucus which can trap pathogens and debris. With the aid of cilia, these harmful agents are remove them from the body. Within the nasal cavity are 3 bumps called nasal conchae, which divide the nasal cavity into three winding spaces called the nasal meatuses.
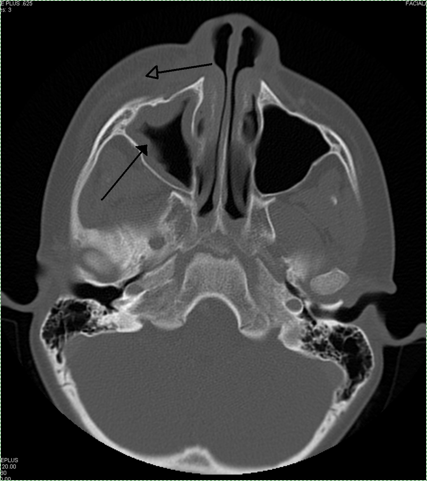
When the para-nasal sinuses become inflamed (known as sinusitis), the small ducts leading to the nasal sinuses may become obstructed. The increase in fluid that accompanies inflammation will then have nowhere to drain, leading to pressure within the sinuses. Furthermore, one response of goblet cells to inflammatory signals is to produce more mucous proteins, which again will have nowhere to drain.